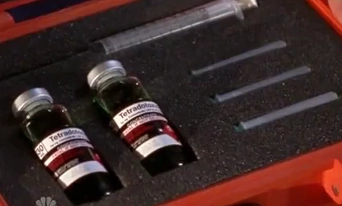
Tetrodotoxin
Tetrodotoxin Pufferfish Extract, a neurotoxin C11H17N3O8 that is found especially in pufferfishes and that blocks nerve conduction by suppressing permeability of the nerve fiber to sodium ions Tetrodotoxin Pufferfish Extract. Tetrodotoxin (TTX) is a potent neurotoxin. Its name derives from Tetraodontiformes, an order that includes pufferfish, porcupinefish, ocean sunfish, and triggerfish; several of these species carry the toxin. Although tetrodotoxin was discovered in these fish and found in several other animals (e.g., in blue-ringed octopuses, rough-skinned newts, and moon snails), it is actually produced by certain infecting or symbiotic bacteria like Pseudoalteromonas, Pseudomonas, and Vibrio as well as other species found in Tetrodotoxin (TTX) is a selective sodium channel blocker nonprotein toxin. The consumption of an organism containing TTX can cause neurological and gastrointestinal symptoms. TTX, widely distributed among marine as well as terrestrial animals, induces dangerous intoxication. This toxin is mainly isolated from the skin, viscera, ovaries, and liver of the pufferfish. The toxin is produced by various species of bacteria, and TTX-bearing animals absorb and accumulate it through the food chain. TTX is commonly used in many laboratories as a pharmacological tool because of its ability to selectively block the sodium channels on the nerve membrane. No antidote is available for clinical use. animals.
Tetrodotoxin Pufferfish Extract (TTX) is a potent neurotoxin responsible for many human intoxications and fatalities each year. The origin of TTX is unknown, but in the pufferfish, it seems to be produced by endosymbiotic bacteria that often seem to be passed down the food chain.
The ingestion of contaminated pufferfish, considered the most delicious fish in Japan, is the usual route of toxicity. This neurotoxin, reported as a threat to human health in Asian countries, has spread to the Pacific and Mediterranean, due to the increase of temperature waters worldwide. Tetrodotoxin Pufferfish Extract
Detection of body fluids
Tetrodotoxin may be quantified in serum, whole blood or urine to confirm a diagnosis of poisoning in hospitalized patients or to assist in the forensic investigation of a case of fatal overdosage. Most analytical techniques involve mass spectrometric detection following gas or liquid chromatographic separation
Tetrodotoxin. The pufferfish has an endosymbiotic (a form of symbiosis in which one organism lives inside the other) bacterium in its body that produces tetrodotoxin, a toxin that is selective for voltage-gated sodium channels. In fact, this bacterium can be found in a variety of marine and terrestrial species in which tetrodotoxin is also found, including the blue-ringed octopus (Bane et al., 2014; Magarlamov et al., 2017). Despite the presence of this dangerous toxin, pufferfish (“fugu”) is a delicacy in Japan. Specially trained chefs purposely leave some tetrodotoxin in the fish they prepare so the consumer can experience the desired side effects of the meal: a tingling sensation in their mouth and a sense of euphoria.
Tetrodotoxin Pufferfish Extract. TTX, for which there is no known antidote, inhibits sodium channel producing heart failure in many cases and consequently death. In Japan, a regulatory limit of 2 mg eq TTX/kg was established, although the restaurant preparation of “fugu” is strictly controlled by law and only chefs qualified are allowed to prepare the fish. Due to its paralysis effect, this neurotoxin could be used in the medical field as an analgesic to treat some cancer pains.Bromazolam for sale USA
Toxicity
TTX is extremely toxic. The Material Safety Data Sheet for TTX lists the oral median lethal dose (LD50) for mice as 334 μg per kg. For comparison, the oral LD50 of potassium cyanide for mice is 8.5 mg per kg,[40] demonstrating that even orally, TTX is more poisonous than cyanide. TTX is even more dangerous if administered intravenously; the amount needed to reach a lethal dose by injection is 8 μg per kg in mice. Tetrodotoxin Pufferfish Extract
The toxin can enter the body of a victim by ingestion, injection, inhalation, or through abraded skin.
Poisoning occurring as a consequence of the consumption of fish from the order Tetraodontiformes is extremely serious. The organs (e.g. liver) of the pufferfish can contain levels of tetrodotoxin sufficient to produce the described paralysis of the diaphragm and corresponding death due to respiratory failure. Toxicity varies between species and at different seasons and geographic localities, and the flesh of many pufferfish may not be dangerously toxic.
The mechanism of toxicity is through the blockage of fast voltage-gated sodium channels, which are required for the normal transmission of signals between the body and the brain. As a result, TTX causes loss of sensation, and paralysis of voluntary muscles including the diaphragm and intercostal muscles, stopping breathing.
Tetrodotoxin Pufferfish Extract
Tetrodotoxin is a sodium channel blocker. It inhibits the firing of action potentials in neurons by binding to the voltage-gated sodium channels in nerve cell membranes and blocking the passage of sodium ions (responsible for the rising phase of an action potential) into the neuron. This prevents the nervous system from carrying messages and thus muscles from contracting in response to nervous stimulation.
Its mechanism of action, selective blocking of the sodium channel, was shown definitively in 1964 by Toshio Narahashi and John W. Moore at Duke University, using the sucrose gap voltage clamp technique.
The association of bacterial species with the production of the toxin is unequivocal – Lago and coworkers state, “[e]ndocellular symbiotic bacteria have been proposed as a possible source of eukaryotic TTX by means of an exogenous pathway, and Chau and coworkers note that the “widespread occurrence of TTX in phylogenetically distinct organisms… strongly suggests that symbiotic bacteria play a role in TTX biosynthesis” – although the correlation has been extended to most but not all metazoans in which the toxin has been identified.
History
The therapeutic uses of puffer fish (tetraodon) eggs were mentioned in the first Chinese pharmacopoeia Pen-T’so Ching (The Book of Herbs, allegedly 2838–2698 BC by Shennong; but a later date is more likely), where they were classified as having “medium” toxicity, but could have a tonic effect when used at the correct dose. The principal use was “to arrest convulsive diseases”.
In the Pen-T’so Kang Mu (Index Herbacea or The Great Herbal by Li Shih-Chen, 1596) some types of the fish Ho-Tun (the current Chinese name for tetraodon) were also recognized as both toxic yet, at the right dose, use as part of a tonic. Increased toxicity in Ho-Tun was noted in fish caught at sea (rather than river) after the month of March.
It was recognized that the most poisonous parts were the liver and eggs, but that toxicity could be reduced by soaking the eggs, noting that tetrodotoxin is slightly water-soluble, and soluble at 1 mg/ml in slightly acidic solutions.
The German physician Engelbert Kaempfer, in his “A History of Japan” (translated and published in English in 1727), described how well known the toxic effects of the fish were, to the extent that it would be used for suicide and that the Emperor specifically decreed that soldiers were not permitted to eat it. There is also evidence from other sources that knowledge of such toxicity was widespread throughout Southeast Asia and India.
The first recorded cases of TTX poisoning affecting Westerners are from the logs of Captain James Cook from 7 September 1774. On that date Cook recorded his crew eating some local tropic fish (pufferfish), and then feeding the remains to the pigs kept on board.
The crew experienced numbness and shortness of breath, while the pigs were all found dead the next morning. In hindsight, it is clear that the crew survived a mild dose of tetrodotoxin, while the pigs ate the pufferfish body parts that contain most of the toxin, thus being fatally poisoned.
The toxin was first isolated and named in 1909 by Japanese scientist Dr. Yoshizumi Tahara. It was one of the agents studied by Japan’s Unit 731, which evaluated biological weapons on human subjects in the 1930s.
On the contrary, there has been a failure in a single case, that of newts (Taricha granulosa), to detect TTX-producing bacteria in the tissues with the highest toxin levels (skin, ovaries, muscle), using PCR methods, although technical concerns about the approach have been raised.
Critically for the general argument, Takifugu rubripes puffers captured and raised in a laboratory on controlled, TTX-free diets “lose toxicity over time,” while cultured, TTX-free Takifugu niphobles puffers fed on TTX-containing diets saw TTX in the livers of the fishes increase to toxic levels.
Hence, as bacterial species that produce TTX are broadly present in aquatic sediments, a strong case is made for ingestion of TTX and/or TTX-producing bacteria, with accumulation and possible subsequent colonization and production.
Nevertheless, without clear biosynthetic pathways (not yet found in metazoans, but shown for bacteria), it remains uncertain whether it is simply via bacteria that each metazoan accumulates TTX; the question remains as to whether the quantities can be sufficiently explained by ingestion, ingestion plus colonization, or some other mechanism.
Symptoms and treatment
The diagnosis of pufferfish poisoning is based on the observed symptomatology and recent dietary history. Symptoms typically develop within 30 minutes of ingestion, but may be delayed by up to four hours; however, if the dose is fatal, symptoms are usually present within 17 minutes of ingestion. Paresthesia of the lips and tongue is followed by developing paresthesia in the extremities, hypersalivation, sweating, headache, weakness, lethargy, incoordination, tremor, paralysis, cyanosis, aphonia, dysphagia, and seizures. The gastrointestinal symptoms are often severe and include nausea, vomiting, diarrhea, and abdominal pain; death is usually secondary to respiratory failure. There is increasing respiratory distress, speech is affected, and the victim usually exhibits dyspnea, mydriasis, and hypotension. Paralysis increases, and convulsions, mental impairment, and cardiac arrhythmia may occur. The victim, although completely paralyzed, may be conscious and in some cases completely lucid until shortly before death, which generally occurs within 4 to 6 hours (range ~20 minutes to ~8 hours). However, some victims enter a coma. If the patient survives 24 hours, recovery without any residual effects will usually occur over a few days. Therapy is supportive and based on symptoms, with aggressive early airway management. If ingested, treatment can consist of emptying the stomach, feeding the victim activated charcoal to bind the toxin, and taking standard life-support measures to keep the victim alive until the effect of the poison has worn off. Alpha adrenergic agonists are recommended in addition to intravenous fluids to combat hypotension; anticholinesterase agents “have been proposed as a treatment option but have not been tested adequately”. Toad vemom for sale No antidote has been developed and approved for human use, but a primary research report (preliminary result) indicates that a monoclonal antibody specific to tetrodotoxin is in development by USAMRIID that was effective, in one study, for reducing toxin lethality in tests on mice.
Potential medicinal use
The deathstalker’s powerful venom contains the 36-amino acid peptide chlorotoxin (ribbon diagram shown). This blocks small-conductance chloride channels, immobilizing its prey. Scorpion venom is a mixture of neurotoxins; most of these are peptides, and chains of amino acids.
Many of them interfere with membrane channels that transport sodium, potassium, calcium, or chloride ions. These channels are essential for nerve conduction, muscle contraction and many other biological processes. Some of these molecules may be useful in medical research and might lead to the development of new disease treatments.
Among their potential therapeutic uses are analgesic, anti-cancer, antibacterial, antifungal, antiviral, antiparasitic, bradykinin-potentiating, and immunosuppressive drugs. As of 2020, no scorpion toxin-based drug is on sale, though chlorotoxin is being trialled for use against glioma, a brain cancer. Tetrodotoxin Pufferfish Extract Tetrodotoxin Pufferfish Extract Tetrodotoxin Pufferfish Extract Tetrodotoxin Pufferfish Extract Tetrodotoxin Pufferfish Extract Tetrodotoxin Pufferfish Extract Tetrodotoxin Pufferfish Extract Tetrodotoxin Pufferfish Extract Tetrodotoxin Pufferfish Extract Mode of action Tetrodotoxin causes paralysis by affecting the sodium ion transport in both the central and peripheral nervous systems. A low dose of tetrodotoxin produces tingling sensations and numbness around the mouth, fingers, and toes. Higher doses produce nausea, vomiting, respiratory failure, difficulty walking, extensive paralysis, and death. As little as 1–4 mg of the toxin can kill an adult. Saxitoxin has a very different chemical structure than tetrodotoxin, but it has similar effects on the transport of cellular sodium and produces similar neurological effects. Saxitoxin is less toxic than tetrodotoxin. Some people, particularly in Asia, consider puffer fish a fine delicacy if it is carefully prepared by experienced chefs. The trick is to get just a small dose to feel mild tingling effects, but not the more serious symptoms of tetrodotoxin poisoning. In the United States tetrodotoxin poisoning is rare, but a recent US report indicated several cases of people catching and consuming puffer fish containing elevated levels of these toxins and suffering the ill effects. Treatment Treatment is supportive and symptom-based. Activated charcoal may be helpful.